Corneal transplant
Have you ever heard of corneal transplantation or even corneal repair surgery? Yes — we are referring specifically to the cornea, the outermost part of the eye, which requires extremely delicate handling. Because of its location, positioned between the complex internal structures of the eye and the external environment, the cornea is highly vulnerable to many diseases.
In certain cases, these conditions progress and lead to permanent corneal damage or irreversible injury. For this reason, in today’s article from Dr. Sherif Momtaz Hegazy’s Center, we will explore corneal transplantation — the definitive treatment option for advanced corneal diseases — along with its advantages, disadvantages, and everything you need to know about the procedure.
Corneal transplant operation
The importance of the cornea
Before learning the details of the corneal transplant procedure, we will highlight the anatomy and function of the cornea.
The cornea is the transparent layer located in front of the iris of the eye. The cornea is dome-shaped with a slight curvature and is characterized by high refractive power.
It works by refracting the light rays entering the eye and then transferring these rays through the internal lens to the retina to complete correct vision.
Accordingly, high transparency of the cornea and a defect-free phalanx shape are very important for vision.
However, it should be noted that the tissues of the cornea of the eye are not capable of self-regeneration, and therefore any problem with it requires immediate treatment, otherwise the problem will worsen and become more serious.
For example, in severe cases of keratoconus or even keratitis, ulcers on the cornea of the eye can develop into untreatable ulcers, and in this case, we will have no option but to perform a corneal transplant.
Corneal transplant operation
Corneal transplantation is defined as a surgical procedure in which the corneal layer is completely removed after it has been damaged or lost its transparency, and then new corneal tissue taken from a donor is transplanted so that the new cornea is characterized by high transparency and good health.
This procedure is considered a delicate surgery that requires high medical and surgical expertise to achieve good results.
It is also widespread, as more than 45,000 patients undergo corneal transplants annually in the United States alone, so what about the situation in Arab countries?
Steps for performing a corneal transplant
Perhaps the most exciting information for most patients is the steps involved in the corneal transplant procedure, where we enter the operating room and accompany the doctor through all the steps and stages of the operation, with each step and movement explained and its details clarified as follows:
- First of all, the doctor thoroughly disinfects the area around the eyes and eyelids to reduce the risk of infection and inflammation.
- Eye anesthesia, either local or general, is used, especially if the patient is a young child or an adult who cannot undergo local anesthesia.
- Using a custom eyelid separator or clip ensures that the eyelids remain open throughout the procedure.
- The cornea is removed by means of a specialized surgical scalpel, either completely or partially, where the doctor makes a circular surgical incision in the center of the cornea.
- Sometimes, depending on the case, the cornea can be removed using a femtosecond laser.
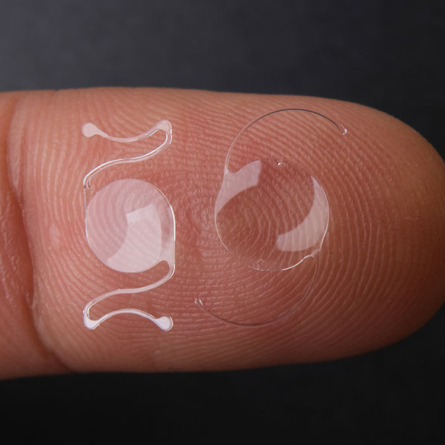
- New tissue or corneal layers taken from a donor using microsurgical techniques are placed in the place of the original cornea and stitched with surgical sutures.
- If the patient also has cataracts, cataract surgery may be performed at this step, in which the cataracts are removed and a healthy lens is implanted.
- An antibiotic medication in the form of eye drops is applied to the eye after the surgical sutures are finished, and the surgery is completed by placing a medical patch on the eye to protect it.
Types of corneal transplant procedures
The term corneal transplantation is not a general and comprehensive procedure at all, but rather it branches out into several highly advanced and precise surgical procedures, the most important of which are:
Full corneal transplant
It is a surgical procedure in which all layers of the damaged cornea are replaced with a new, complete, healthy, and problem-free cornea.
·DALK corneal top layer transplant
In the procedure of superior stratified corneal transplantation, only the upper outer layer of the cornea of the eye is replaced, specifically the stroma and epithelial layers.
Scientifically, this procedure is called deep anterior lamellar corneal transplantation, and it targets patients with superficial corneal problems such as advanced keratoconus.
In this procedure, only the upper layers of the cornea are treated without affecting the endothelial layers, and therefore there is no risk of immune rejection.
As for the surgical procedure, air is injected into the cornea of the eye in order to separate the layers of the cornea and remove only the outer and middle layers and replace them.
Here the surgery is short and brief compared to a total corneal transplant, the recovery period after it is very quick, its complications are limited, and the duration of use of steroid eye drops is short.
Endocorneal transplant
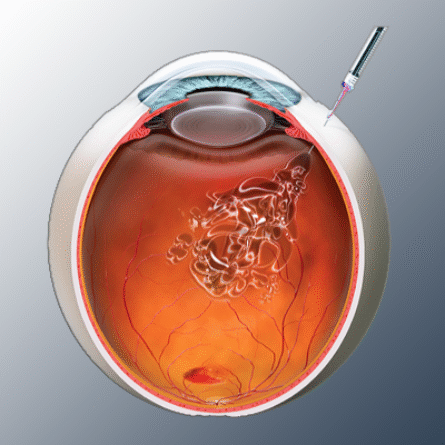
This type of corneal transplant targets the lower layers of the cornea, specifically the endothelial layer and Descemet membrane.
Endothelial corneal transplantation often treats problems of infiltrative keratopathy, hereditary corneal problems, or corneal damage following cataract surgery.
As for the details of the endothelial corneal transplant surgery, it is done in the usual steps, but the cornea is not completely removed. Rather, the endothelial layer is scraped off and removed, and in its place, an endothelial layer taken from a donor is placed. Often, the surgeon injects air into the eye to ensure that the tissues stick together.
The following are the risks of corneal transplant surgery
Despite the high safety rating and large success rate of corneal transplant surgery, the risk still exists and cannot be ignored.
In this surgery, the delicate corneal tissues of the eye are dealt with, and any small mistake could cause serious complications.
This is where the importance of consulting Dr. Sherif Mumtaz Hegazy, the best ophthalmologist in Egypt, lies, to perform the operation with the highest degree of surgical precision and efficiency. The risks of this procedure include the following:
- Astigmatism or irregularity of the corneal surface.
- Cataracts, also known as white water or cataracts, cause blurred vision.
- Possible bacterial and viral infections can be treated with antibiotic eye drops.
- Opacity in the new tissue of the cornea requires corrective action.
- Bleeding in the layers of the skin or eyelids is temporary and disappears within a short period.
- Abnormal growth of blood vessels on the cornea of the eye.
- High eye pressure, also known as glaucoma.
- Retinal detachment that requires a new treatment procedure.
- Swelling of the cornea of the eye as a symptom of inflammation or normal swelling that disappears within a short period of time.
- Immune tissue rejection, an automatic reaction of the body, is treated with autoimmune suppressants or corrective surgery.
Patients who are candidates for corneal transplantation
Corneal transplantation is not a simple procedure that a patient can resort to if they have minor vision problems.
It is an advanced surgery in which one form of human organ transplantation, namely the cornea, is performed, which means that it involves many risks and complications.
Therefore, Dr. Sharif Mumtaz Hijazi only resorts to this procedure when he finds it to be the final treatment option for a patient for whom none of the other corneal disease treatment procedures are effective.
In general, the supervising physician is the only one qualified to refer the patient for this procedure according to specific conditions and standards.
Among the most important medical conditions
Among the most important medical conditions and patients who are candidates for corneal transplant surgery, we mention the following:
- Deteriorating keratoconus that does not respond to corneal cross-linking with riboflavin, corneal ring implantation, or any other procedure, and the morphological deformity of the cornea develops and it loses its transparency completely.
- Corneal effusion that does not improve after cataract surgery and the resulting loss of corneal transparency.
- Chronic infection of the cornea of the eye that causes permanent damage to it, in addition to bacterial, viral and fungal growth that causes corneal ulceration later on.
- Permanent damage to the cornea of the eye resulting from direct injuries to the eye or exposure of the cornea to chemical damage.
- The inner cells in the endothelial layers of the cornea die as a result of Fuchs’ atrophy, leading to vision loss and corneal swelling.
- The immune rejection of the transplanted tissue in the cornea of the eye is a result of previous transplant surgeries, and therefore corrective corneal transplantation should be performed.
Recovery phase after corneal transplant surgery
After undergoing corneal transplant surgery, the patient will go through a relatively difficult period in terms of pain, care, and visual symptoms as well.
The results of improved vision after the operation are delayed and may appear after several weeks or sometimes months.
The patient is prohibited from driving a car on the day of surgery and for the few days following it because his vision is still unstable.
Appointments for doctor check-ups are often scheduled during the first day, the first week, and the first month after surgery to ensure the patient’s eye health and the excellent results of the surgery.
Here, the patient must use the prescribed eye drops and ointments for the period specified by the doctor.
It is also normal to feel tingling and prickling in the first days and weeks after the operation.
The patient is required to take full care of his eyes and protect them from any external factors or intentional movements for a very long period, sometimes up to a full year.
However, if the patient notices unusual symptoms in his eyes, such as blurred vision, light sensitivity, blood pooling in the eyes, or severe redness, then there is a possible risk of immune rejection, which requires going directly to an eye medicine and surgery center.
Key guidelines after corneal transplant surgery
The period following a corneal transplant is relatively challenging, during which the patient may face several difficulties in caring for and protecting their eyes, managing the side effects of the surgery, and other related issues. However, following the doctor’s instructions and medical guidance after the procedure is extremely important and must not be neglected.
Some of the most important medical guidelines to follow during the first few weeks after the surgery include:
- It is necessary to wear the eye patch while sleeping, bathing, or being in polluted places.
- Lying on your back and not sleeping on your side during the first few days after the operation is prohibited, and sleeping on your stomach is strictly forbidden.
- Wear sunglasses when leaving the house, especially on sunny days and in places with bright lights.
- Therapeutic eyeglasses may be prescribed for astigmatism that may occur after corneal transplantation.
- Use eye drops and therapeutic ointments at the correct time and in precise doses because they protect against the risk of immune rejection.
- Avoid rubbing or scratching your eyes, or applying creams or cosmetics around or inside them.
- Abstain completely from smoking cigarettes, hookahs, or even exposure to drafts.
- Avoid straining your eyes by looking at electronic devices such as mobile phones and televisions.
Corneal transplantation with stem cells
The corneas suitable for transplantation into the eye are usually obtained from the cornea bank in the United States of America, where there are stores of healthy corneal tissue that has been obtained under specific and strict conditions and has a clear expiry date and is delivered to the receiving medical center with high accuracy.
However, some patients do not accept the idea of receiving a new cornea from a deceased donor, so the idea of cornea transplantation with stem cells arouses their curiosity.
Indeed, in recent years bioengineering has been employed to guide stem cells to create a complete cornea that is implanted in the affected eye.
This is done by taking stem cells from a healthy cornea, multiplying these cells to a certain number, and then implanting and sewing them into the area of the damaged cells.
But despite this great progress in the field of corneal transplantation, these techniques are still under research and have not been included as approved treatment procedures.
The difference between corneal transplantation and corneal grafting
The concept of corneal transplant surgery is often confused with the corneal grafting procedure, and patients seek a precise explanation of these two procedures, which we will explain to you in the following lines:
Corneal transplantation is a delicate surgery in which the entire cornea of the eye is replaced with a healthy cornea that can be obtained from a donor under specific conditions. Corneal transplantation is performed in cases of advanced deformities and problems in the front and back layers of the cornea of the eye, and the recovery period after this operation can reach a full year or even 18 months in some cases.
Corneal grafting is also referred to as partial corneal transplantation, in which only certain layers of the cornea—either the anterior or posterior layers—are replaced with healthy tissue, depending on the location of the damage. In this case, the eye or corneal disease has affected only specific layers rather than the entire cornea. Therefore, partial-layer corneal transplantation is considered a safer option. The recovery period after this procedure is approximately 4 months.
Best cornea doctor in Egypt
Dr. Sherif Momtaz Hegazi is considered the best ophthalmologist in Egypt for performing total and partial corneal transplant surgery with high professionalism.
His medical center has been equipped with the latest technologies and equipment used in this procedure and other eye surgeries, which ensures the highest success rates, thanks to God Almighty.
Moreover, Dr. Sherif Hegazy has gained unparalleled experience through his continuous pursuit and work in leading medical institutions such as:
Royal College of Surgeons – International Council of Ophthalmology – University of Tübingen – Institute of Research in Ophthalmology and others..
He distinguished himself in every place he actually was, as he embarked on this path after obtaining a master’s degree from Cairo University and then a degree in ophthalmology from Al-Qasr Al-Aini University.
He subsequently achieved distinction from the International Council of Ophthalmology, which qualified him for an international scholarship. He also completed an advanced fellowship at Tübingen University in Germany in the Department of Retina and Vitreous Surgery, and was appointed as a trainer and international fellow at the Research Institute of Ophthalmology in Egypt, as well as an international examiner for the Royal College of Surgeons in the UK.
His research achievements are so outstanding that his scientific and medical studies have become highly referenced, and his international lectures and presentations attract the attention of ophthalmologists and ophthalmology students from around the world.